Written by Dr. Mackenzie Chadderdon, PT, DPT
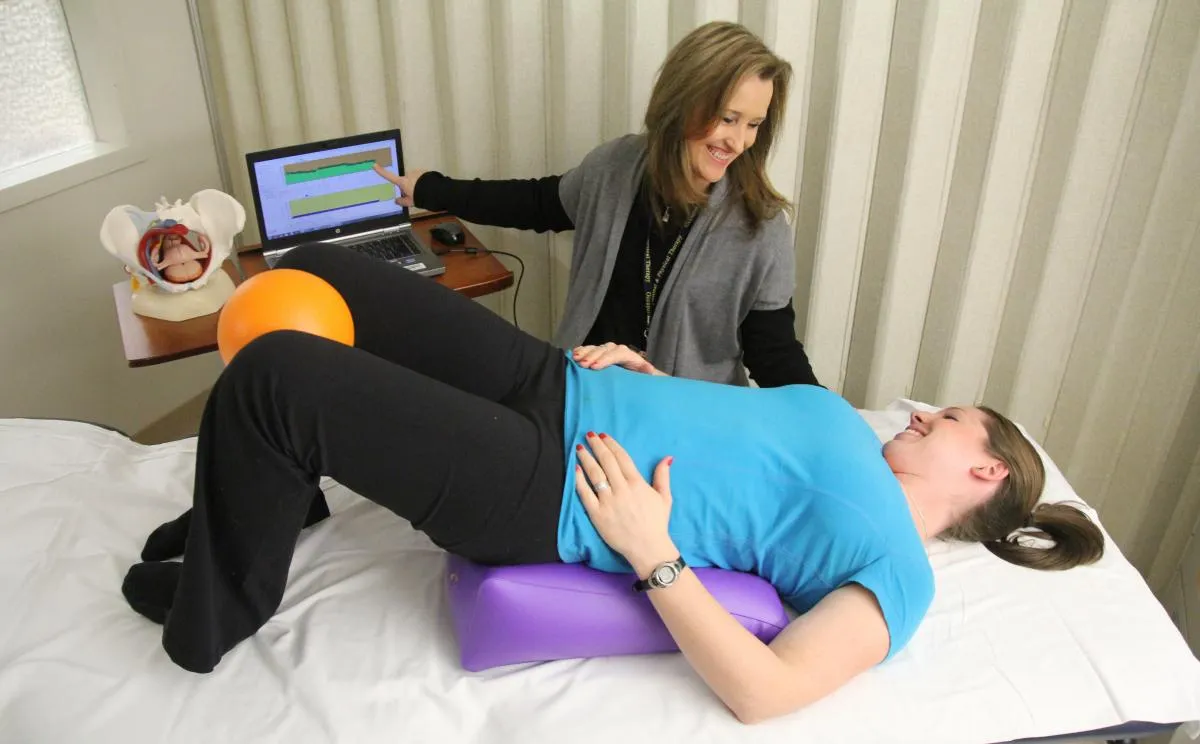
Pelvic floor physical therapy is an effective treatment approach for managing pelvic floor dysfunctions such as urinary incontinence, pelvic pain, and prolapse. These conditions stem from weak, tight, or imbalanced muscles in the pelvic region, and therapy focuses on improving strength, flexibility, and coordination. At the mention of pelvic floor physical therapy generally these and other pregnancy or postpartum related things may come to mind. However, achieving optimal pelvic health involves more than just manual or exercise related physical therapy treatment; dietary habits also play a significant role. Nutrition can influence bowel habits, inflammation, and even muscle function, which are all critical factors in pelvic floor health. Addressing diet alongside pelvic floor muscle function can therefore enhance results and provide a more holistic approach to pelvic care.
One of the most important aspects of diet for pelvic health is fiber intake. Consuming adequate amounts of fiber helps maintain regular bowel movements, which is vital for preventing straining during defecation—a common cause of pelvic floor dysfunction. Chronic constipation can place excessive pressure on the pelvic floor muscles, leading to weakness or even prolapse over time. A fiber-rich diet, which includes fruits, vegetables, whole grains, and legumes, can help prevent constipation, reducing the risk of further pelvic strain. For individuals undergoing PFPT, managing constipation through diet can support the rehabilitation of the pelvic muscles by alleviating one of their primary stressors.
Constipation doesn’t just strain the pelvic floor; it often leads to bloating, which can further aggravate pelvic discomfort. Bloating is a common symptom in many of our patients. It creates additional pressure in the abdominal and pelvic regions, making it harder for the pelvic muscles to function optimally. Certain dietary choices, such as eating high-fiber foods slowly and avoiding excessive amounts of gas-producing foods like beans or carbonated drinks, can help reduce bloating. Balancing fiber intake with plenty of water is essential, as fiber without adequate hydration can actually worsen constipation and bloating. Proper hydration helps soften stools, making it easier to pass them without undue stress on the pelvic muscles.
Fluid intake is another critical factor to consider in pelvic floor health. Drinking enough water not only supports digestion but also helps maintain bladder health. Dehydration can lead to concentrated urine, which irritates the bladder and can exacerbate symptoms of urinary urgency or frequency, both of which place additional strain on the pelvic floor muscles. On the other hand, overconsumption of bladder irritants like caffeine or alcohol can worsen these symptoms. A well-balanced fluid intake, primarily consisting of water, can support bladder health and reduce unnecessary pelvic floor stress.
For those experiencing pelvic pain, especially conditions like interstitial cystitis or irritable bowel syndrome (IBS), identifying and avoiding specific dietary triggers can be crucial. Certain foods, like spicy foods, citrus, or artificial sweeteners, may exacerbate pelvic pain and inflammation. By working with a healthcare provider or nutritionist, individuals can identify foods that contribute to inflammation or irritation, making it easier for the pelvic muscles to relax and function normally. Reducing inflammatory foods and focusing on anti-inflammatory options like leafy greens, healthy fats, and lean proteins may further enhance pelvic floor physical therapy’s benefits.
Incorporating healthy fats and adequate protein into the diet is also essential for muscle repair and overall pelvic health. The pelvic floor muscles, like any other muscle group, need proper nourishment to recover and strengthen. Omega-3 fatty acids, found in fish, nuts, and seeds, can help reduce inflammation, while lean protein supports muscle repair and growth. A balanced diet that includes healthy fats and proteins ensures that the pelvic floor muscles have the nutrients they need to heal and function effectively in response to physical therapy.
Pelvic floor physical therapy is key to restoring pelvic function, and as providers who care for you as a whole person and are looking for all avenues to improve your life it’s essential as a provider to consider diet as part of a comprehensive approach to pelvic health. Managing fiber intake, avoiding constipation, reducing bloating, and maintaining proper hydration all contribute to the optimal functioning of the pelvic floor. By aligning dietary habits with physical therapy, individuals can accelerate their progress and improve their overall quality of life, ensuring long-term pelvic health and function.
References:
1. van der Schoot A, Et. Al. The effect of fiber supplementation on chronic constipation in adults: An updated systematic review and meta-analysis of randomized controlled trials. The American Journal of Clinical Nutrition. July 11, 2022. Accessed September 25, 2024. https://www.sciencedirect.com/science/article
2. Nap A, de Roos N. Endometriosis and the effects of dietary interventions: What are we looking for? Reproduction & fertility. May 30, 2022. Accessed September 25, 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9259892/.
3. Curillo-Aguirre CA, Gea-Izquierdo E. Effectiveness of pelvic floor muscle training on quality of life in women with urinary incontinence: A systematic review and meta-analysis. Medicina (Kaunas, Lithuania). May 23, 2023. Accessed September 25, 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10301414/.